bitin' list
everything you don't want to google about rabies
Happy World Rabies Day!
Let’s do a fun little poll. Have you ever received a rabies vaccination?1
It Happened To Me: I Ghosted My County Rabies Man
When I was eighteen, I was working at a local vet as an Inpatient Care Technician, which means that I took care of the dogs being boarded in the kennel. My job was to feed them, clean up their pee, make sure they got to run around outside for at least 15 minutes, and stalk them to try to get pee samples.
One day I was trying to get a poodle outside during a thunderstorm, and the dog freaked out. I moved too suddenly to grab her, and she bit me on the shoulder. I was entirely to blame for the situation, and because I was young and an idiot, I went up front and showed off my cool bloodstains to the office manager, who freaked out, made me sign six forms releasing the practice of liability, and then went digging for the dog’s rabies forms.
Surprise! Millie’s vaccination was expired.
Thirty minutes later, the kennel manager was driving me to the health department for my first rabies shot. Contrary to myth, it wasn’t in my butt, thigh, or stomach; I got the first and second shots in my upper arm, near the bite. I never ended up getting my third shot, because I went back to college before it was due, so my boss wasn’t able to physically force me into compliance.
The rabies man hounded (lol) me after that, calling me almost every other day to track how I was feeling, did I have symptoms, was I itchy, did I have a fever? I started ducking his calls because I was sick of talking to him. I was in college, dude: It is not cool to be on first-name basis with the rabies man.
As you may have guessed, I didn’t get rabies from either of these adventures. I was never really in danger of getting rabies, because domestic canine rabies rates are extremely low in the U.S. But I wish I could reach back in time and slap my younger self for being such a little shit about it. Because in case you didn’t know, rabies fucking sucks.
In case you don’t know, in honor of World Rabies Day, I present you with:
Things I Find Interesting About Rabies
Rabies is not just a fear of water.
Rabies is a neurological condition that impacts most mammals2 and is transmitted via the exchange of bodily fluids, most commonly saliva and blood. The vast majority of transmissions are through bites between animals, or from animals to humans. To knowledge, no human-to-human bite transmissions have been recorded, but it is possible to spread between humans via organ transplants.3
Infection often begins with flu-like symptoms setting in within weeks of the bite, as well as pain or burning around the wound. As the disease progresses, it causes inflammation of the brain, which can lead to paralysis, hallucinations, agitation and occasionally a fear of water. The latter is because rabies may cause muscle spasms in the larynx, making it painful and sometimes impossible to swallow. This causes an abundance of saliva, resulting in the classic “foaming at the mouth” symptom.
Eventually the infection spreads to the heart, kidney, and liver, causing multiple organ shut down, which results in death.
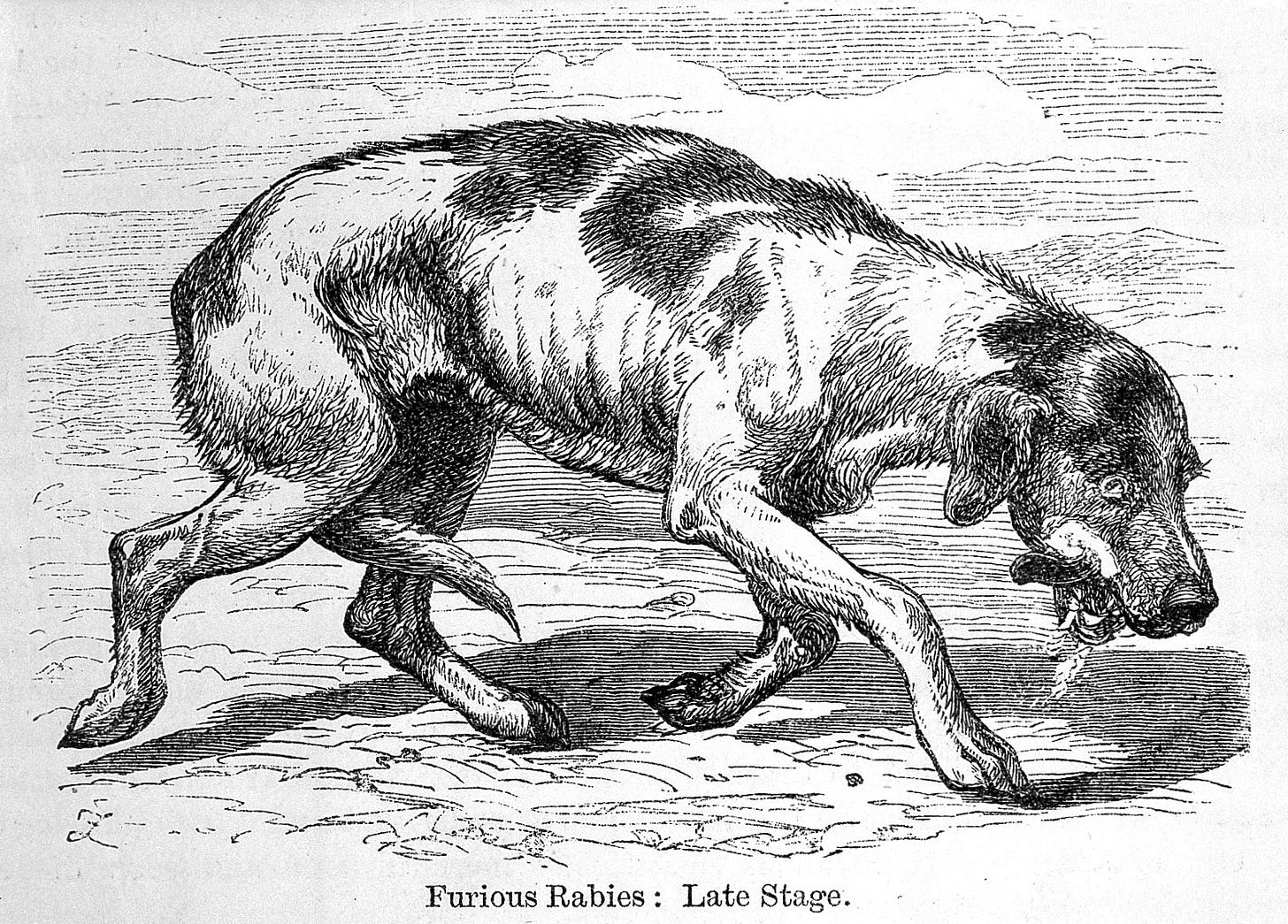
There are two forms of rabies, which appear in both human and animal victims:
Furious rabies which presents with aggression, hallucination, lack of coordination and fear of water. The most common cause of death in furious rabies is respiratory arrest, usually within days of infection.
Paralytic rabies takes longer to fully manifest, and accounts for about 20% of human cases. In paralytic rabies, infected will experience gradual muscle paralysis, and eventually a coma. Experts believe that paralytic rabies is underreported, because the populace is not as familiar with these symptoms.
Rabies is virtually incurable.
Rabies causes almost 60,000 human deaths a year across the globe, and about 40% of victims are children. Once someone enters active rabies, defined as symptom onset, there is no scientifically proven way to beat the infection.
Less than 50 people worldwide have been known to survive rabies. The most famous case is Jeanna Giese, who was just a teenager when she was bitten by a bat in 2004. Geiss was placed into a chemically-induced coma while receiving antiviral medications to encourage her body to produce antibodies. Giese survived, and though she did require substantial rehabilitation, she is still alive 20 years later, and even gave birth to two healthy children.
The method that saved Giese has been dubbed the "Milwaukee protocol” and the physician who created it—an emergency physician in Milwaukee who had never treated a rabies case before—claims that 18 more patients have been saved with this technique. However, there is no published data demonstrating this. Actually, the opposite.
Over the last 20 years, there have been 64 reported cases where the Milwaukee protocol was attempted, and failed. Even those who have temporarily recovered have subsequently passed due to neurological or medical complications stemming from the rabies infection. Other survivors of the protocol are believed to have not actually had rabies infections at all.
Other approaches have been moderately successful, though. At least 34 people have survived rabies infection, largely in India, thanks to robust, critical care—the same approach that helped save the first rabies survivor in 1970. In that case, a 6 year-old boy (also bitten by a bat) was able to survive infection thanks to constant monitoring, addressing complications, and ultimately a tracheostomy.
One paper I found, which debunks the protocol, includes one of the most scathing conclusions I’ve ever read in academic literature.4
Continued repetition of the Milwaukee protocol in multiple versions over about 20 years has failed to show efficacy and has actually served to impede progress for the development of effective therapy for human rabies. Most cases of human rabies occurring in resource-rich countries are encountered by physicians without expertise in rabies who are aware of the poor prognosis in rabies and reach out to or are directly contacted by the main proponent of the Milwaukee protocol, who claims to have had multiple successful cases using this approach. There is little credible evidence of benefit beyond the index report and it is now time that the Milwaukee protocol be abandoned. New approaches need to be taken based on scientific advances in the field rather than endless repetition of this flawed and unsuccessful approach.
Rabies is preventable
So, yes. Rabies is basically fatal. But it’s completely preventable with the use of pre- and post-exposure prophylaxis vaccines.
First discovered by Louis Pasteur in 1885, the rabies vaccine has proven to be one of the strongest, most reliable vaccines in medical history. The margin of failure is extremely low—and since being introduced into the United States in 1970, there has never been a single rabies death in a case where the patient received timely post-exposure vaccination.
Today, over 29 million people worldwide receive the human rabies vaccine annually.
U.S. rabies is on the rise.
Although canine rabies has essentially been eradicated since the 1970s, thanks to vaccination campaigns and requirements, every state in the U.S. still has some rabies presence. About 4,000 animal rabies cases are reported each year, along with fewer than 10 human deaths. These days, transmission is most likely to come from bats, racoons, skunks, foxes, or feral cats.
In the last 12 months, six rabies-related deaths have been reported in the United States, making it the deadliest rabies year in recent history. Over 15 outbreaks have been reported across the U.S., and this summer health officials issued warnings in Nassau County, NY, Cape Cod, and parts of Alaska, Arizona, California, Indiana, Kentucky, Maine, North Carolina, Oregon and Vermont. Residents who come into contact with wild animals in those areas should be cautious and seek medical aid immediately if bitten.
Why? As with everything, the answer is: climate change, environmental erosion, and politics.
In an era of increasing vaccine skepticism and ever-expanding development, wild animals are being displaced into human communities more than ever, and households pets without vaccinations are more susceptible. Natural disasters related to climate change, such as wild fires, are also forcing animals out of their environments, causing them to live in much closer quarters with each other, as well as humans.
Please, for God’s sake, vaccinate your pets. I swear to you on my life that your dog will not get autism.
Poor rural communities have the worst rabies infection rates
Although rabies is present on every continent except Antarctica, in most areas your risk of infection is low. However, rabies infections—particularly canine rabies—disproportionately impact bite victims in India, Africa and East Asia. India alone makes up almost a third of global rabies deaths.
The problem is multifaceted, according to experts. First, India has a huge population of stray dogs, but does not have state-funded monetary support for a wide-spread vaccination campaign. Cost also impacts the accessibility of prophylactic vaccines. As of 2018, the average estimated cost of rabies post-exposure prophylaxis (PEP) was US$ 108 (along with travel costs and loss of income), which can be a financial burden on those earning US$ 1–2 per person, daily, per the World Health Organization.
A lot of sources claim that Puppy Pregnancy Syndrome (PPS) is one of these cultural barriers that has made rabies so prolific in India. PPS, is a type of mass hysteria, essentially causes people to believe that they have become pregnant with puppies following a dog bite.
The Wikipedia entry for rabies attributes PPS to why parts of rural India don’t seek vaccines. Although I have found documentation that this is a real syndrome, I can’t find any peer reviewed sources citing that this is a wide-spread issue beyond one small village in West Bengal.
So while this is a fascinating bit of trivia, I don’t think PPS can at all be credited as a key factor in India’s rabies rates. Far more realistically, rural bite victims don’t seek vaccines because of a lack of accessible care or funds, as well as a general distrust of “Western” medicine due to the knock-on effects of Imperialism, colonization and racism. But puppy pregnancy syndrome is so much more enjoyable to talk about.
Vaccination campaigns work.
Like a lot of diseases, rabies is completely possible to eradicate, if we choose to.5
According to Mission Rabies, a U.K.-based program of the Worldwide Veterinary Service (WVS) which seeks to eliminate global rabies, the easiest way to prevent transmission is to support vaccination programs for wild dogs and other animals, educate local populations, and investigate potential outbreaks.
Experts know that vaccination campaigns work; leaving out oral vaccines in bait traps has been shown to reduce transmission rates dramatically. Campaigns to encourage domestic pet vaccination have eradicated the disease in multiple counties, and wide-spread education has kept human death rates low.
Canine rabies is essentially eradicated in the U.S., and the United Kingdom has been almost entirely free of rabies since the 1920s. Sweden and Norway have been rabies-free for even longer, while Italy achieved a rabies-free status thanks to an extensive wild animal vaccination campaign in the mid-2000s.
Even in areas with high infection rates, organized campaigns have been able to make a drastic difference to quality of life.
In 2024, The Nagpur Municipal Corporation (NMC), in collaboration with Mission Rabies, vaccinated over 20,000 dogs in Maharashtra over the course of one month. A small town in Tamil Nadu managed to achieve 100% rabies vaccination and seven years of no human deaths thanks to a week-long vaccination campaign and longitudinal education. In Goa, human rabies has almost been eradicated thanks to education, vaccination and data-driven technology campaigns, and last year Cambodia successfully vaccinated over 230,000 dogs with support from Mission Rabies.
YOU can stop the spread of rabies!
Mission Rabies is always in need of donations, which go directly to supporting efforts like the ones listed above. They’re having a concrete, actionable impact on rabies eradication, thereby improving life for humans and animals alike.
In honor of World Rabies Day, I’m making a donation to Mission Rabies, and would highly encourage you to consider it as well. My birthday is tomorrow, after all.
If you’re not in a position to donate, you can still give me a gift by reading, liking, and sharing this Substack, and becoming really annoying to all your friends about rabies.
Also, you can follow me on my new writing instagram, @hopeanna.writes.
Until next time,
the hypocrite who never completed her rabies vaccination
Treat thyself to the song that got me thinking about this particular issue.
Except for Virginia opossums, because their internal temperature is too low to make the disease happy.
Last year, a Michigan resident died after receiving a donated kidney that was infected with rabies. This has happened four times since 1978, largely because the rabies infection was undiagnosed or had not become symptomatic in the donor at the time of death.
Alan C Jackson, Demise of the Milwaukee Protocol for Rabies, Clinical Infectious Diseases, 2025;, ciaf157, https://doi.org/10.1093/cid/ciaf157
Cough, cough, TB.



The way I would be using “it’s my latent rabies” as an excuse for my bad behaviors if it was I bitten by the poodle…